Abstract:
This study examines the implementation and assessment of a back-referral initiative within a teaching hospital, specifically focusing on the Vardaan Referral unit at SRMSIMS, Bareilly. Referral systems are vital components of healthcare networks, facilitating patient movement between different tiers of healthcare facilities. However, India’s current linear referral system encounters obstacles due to factors such as workforce shortages, infrastructure deficiencies, and protocol non-adherence. The Vardaan center was established to streamline referral services and deliver comprehensive care to patients referred from surrounding areas. The objective was to evaluate the initial performance of the Vardaan Referral unit. The study delineates the setup of the Vardaan center, patient referral procedures, and provided services, encompassing counseling and post-referral follow-up. Case studies illuminate the operational dynamics of the Vardaan center and its impact on patient well-being. Discussion underscores the significance of efficient referral systems in bridging healthcare infrastructure gaps, emphasizing the importance of clarity, communication, and adherence to protocols across all healthcare levels. The study concludes that the back-referral system concept is feasible in teaching hospitals through Community Medicine department outreach centers, with a focus on enhancing patient engagement and satisfaction.
INTRODUCTION:
In any healthcare system, referral system at all levels is used to facilitate flow of patients across health facilities. It makes cost-effective use of higher-level hospitals and peripheral health care services, if practiced efficiently. Thus, it improves the access of the population to better quality clinical care. Referral process involves physicians’ decisions about its need, selection of the receiving facility and interactions with it. Inefficient referral decisions and communication affect the quality and cost of care 1- 4.
Referral does not mean only the forward referrals. Downward, (backward) referrals is also of equal importance. As per this concept, the patients treated at the receiving facility, may be referred with the necessary follow-up advice to the original initiating facility (lower-level health care center). It requires clear communications in both the directions, forward, describing the health problem to the receiving facility and backward, information back to the initiating facility describing the actions to be taken with follow up advice. The aim is to assure that the patient receives optimal care at each level of the system1- 4.
Ideally, as per a linear referral system, the access to hospital care should be through primary health centers only, except for emergency situations. Unfortunately, in real life situations, a different scenario is observed at ground level in India. Linear referral system does not work. Any patient can go anywhere, irrespective of the level of existing architectural hierarchy in the health care system without any referral. There is usually, no formal control on the process.
It exerts a huge burden on the higher-level facilities. Usually, it is seen that many patients with minor illnesses reach the outpatient departments (OPDs) of even the tertiary care centres. Ideally, these patients can be easily tackled at the lower level health facility at lower overall cost to the client and the health system, i.e., they do not need to be referred to a higher center.
Causes of failure of linear referral system in India are many, e.g., 1. Lack of skilled and motivated manpower, especially at secondary level. 2. Inadequate infrastructure in the PHCs. 3. Non- adherence to the referral guidelines. 4. Minor cases go directly to a higher level health facility. 5. Lack of accountability at each level for controlling unnecessary referrals. 6. Non-availability of universal health cards like that used in developed countries, where the health facility for primary treatment or screening is indicated for a particular population. No patient can consult a higher level health facility without being referred by the primary treatment facility1- 4.
In this context, the present pilot study attempted to operationalize and evaluate the back referral concept in a teaching hospital
Through their rural and urban training centres of the Community Medicine Departments, all medical colleges in India provide free medical services to the population in the peripheral areas. Now, as per the National Medical Commission guidelines, medical colleges provide exposure to medical students to community/ family health in their initial years 5.
Community Medicine Department of Shree Ram Murti Smarak Institute of Medical Sciences (SRMSIMS), Bareilly, also provide free medical OPD and referral services to the general population in rural / urban areas through Family Adoption Program, hospital on wheels, telemedicine bus and telemedicine center. To coordinate the referral services to the patients seen at these centres, the Chairman and the Director Administration SRMSIMS launched Vardaan referral system management unit on 16th September 2022. It was a unique concept of recycling and minimizing waste, as the centre was housed in a used freight container redesigned as a work-station. It is operated by the Community Medicine Department. The main aim of the Vardaan centre is to channelize the referral system services efficiently and to provide adequate care to the patients referred from the catchment areas of the Department of Community Medicine.
Objective:
To evaluate the initial functioning of Vardaan Referral unit at SRMSIMS, Bareilly
Material and methods:
SRMSIMS hospital is NABH accredited 1200 bed super-specialty tertiary care hospital. It provides a wide spectrum of clinical services to the community. Vardaan center is located opposite to gate 2, at the entrance of SRMSIMS. It is manned by a team comprising of faculty, intern, medical social worker, and a ward boy. This center is housed in a freight container that has been converted in to a cabin (dimensions -12.8 x 2.4 X 2.6 meters). The center is equipped with a reception counter for registration purpose. Facility of pulse, weight and blood pressure measurement, and an examination bed is also there. The center is also connected to the department by a tele-camera, for monitoring by a senior faculty of the Department of Community Medicine.
A team of faculties, post-graduate students and medical social workers provide preventive, promotive and curative health services to the community through Rural / Urban health training center, mobile telemedicine bus, Bhairpura telemedicine center.
The patients are first seen in the general OPDs of these units and referral is made to Vardaan center, SRMSIMS, if needed, using colour coded paper slips (pink, yellow and white). All relevant information regarding the patient, medical history and need for the referral mentioned by the treating doctor is documented in the referral form. The pink colour paper slip is kept at the centres with the doctor for record maintenance; yellow and white paper slips are given to the referred patients.
When a patient reaches the Vardaan centre, the yellow paper is to be submitted at the registration counter for medical record and tracking purpose. Medical history anthropometric measurements, blood pressure, pulse are taken and documented. The patients are sent with the white colour coded paper slips to specialized OPDs escorted by a peon.
Weekly tele-calling is done by the Vardaan center team with the referred patients to enquire about their health status when they reach back to their homes after having consulted a specialist in the hospital.
All patients referred via the Vardaan centre are eligible for discounts (10% on medicines / investigations; 15% on bed charges)
All subjects for this study were told about the nature of this study. Their consent was taken.
Results: A total of 313 patients have reported till now (Table 1). By and large, they were satisfied about the health services provided to them. Most of them were willing to visit again. Following case studies illustrate the functioning of the Vardaan center.
Case study – 1
A 36 Yrs thin built anaemic Muslim illiterate housewife from area B went to Telemedicine Center with a clinical history of headache / insomnia / loss of interest in work / anorexia / weight loss of 5 kg for last 3 months. She also reported feelings of sadness, depression and suicidal tendency. From there she was referred to Vardaan center in October 2022 for counseling and further treatment. Over there, detailed history was taken by Dr Ruchi. Patient’s counseling was also done by her ensuring confidentiality. .
It emerged that the patient was asymptomatic few years back. She started having headache all through the day associated with insomnia and irritation. She complained of depression and hopelessness. She often wanted to commit suicide. She gave a history of family stress associated with domestic squabbles from last 2 years. She had been married for 17 years and had 3 children. She lived in a joint family. Her husband was a daily wager.
There was also a history of similar complaint 12 years back; medications were prescribed by a private practitioner. This was continued for one year. She discontinued the medicine when she felt symptomatic relief.
She was motivated by Dr Ruchi for building her confidence to live a healthy and stress free life. After the session, the patient felt relieved. She was sent to psychiatry department for further treatment. The concerned doctor was informed about the case and was requested to give appropriate appointment for her.
For rehabilitation and complication prevention, weekly tele-calling to the patient was done from Vardaan center to analyze her progress and feedback.
She is regularly being motivated to visit her treating doctor of Psychiatry department SRMSIMS through Vardaan center and not to miss her prescribed dose/time.
Advice given:
- a) Patient: She was advised to regularly visit Vardaan center for counseling; adhere to the drug regimen. She was also advised for periodic examination and follow up; Regular diet, sleep; Listen to devotional music songs; Involve in creational activities (silai bunai –zari karchovi) for avoiding stress and as a part of vocational therapy.
- b) Family: Maintain calm and peaceful atmosphere at home; Family Members were informed about the critical condition of the patient and further complications; They were advised to make efforts to solve the family issues to avoid domestic fights and stress; They were advised to motivate the patient for periodic checkup and follow up; They were advised to give plenty of time to make her happy and not to neglect her; Not to panic or shout on her for mood swings. They were advised to divert her mind to other issues.
- c) Community: Department of Community Medicine team of faculties, post-graduate students and medical social workers were directed to identify the cases of depression in the community and motivate them to seek treatment; they were asked to exhort people to avoid labeling mental depression and psychotic illness as “SOCIAL STIGMA” Current status (progress):
The patient is fully satisfied with the ongoing treatment of the Psychiatry Department, SRMSIMS. She is feeling calm and happy. She found her interest back in doing her household work; she sleeps properly and is stable on drugs.
Case study – 2
A 38 yrs old literate average built Hindu lower middle-class housewife of area R living in a nuclear family was referred from UHTC center to Vardaan Center in March 2023. Her age at marriage was 21 years. She was apparently asymptomatic few years ago. She separated from her husband 8 years back. Then she started living with her parents and her 2 children at parental home.
The problem started when she complained of feelings of depression for last 6 months; headache and weakness for last 1 month anorexia and insomnia for last 15 days. These are linked with unemployment and the associated financial stress from 1 year.
At Vardaan center, detailed counseling was done by the lead author. The patient was advised to do a short vocational course to earn her livelihood and confidence (short computer course, sewing school, teaching job at kindergarten). She was advised to be regular with her diet and sleep. Counseling was done to convince her to listen to relaxing music / songs.
Further, she was sent to the main hospital for requisite treatment.
She was diagnosed with depression. She appeared anaemic on general examination. She was treated with general medications for anaemia and dietary advice. She was advised to adhere with the prescribed medicine and the advice for follow up.
For rehabilitation and complication prevention, weekly tele-counselling with the patient was done from Vardaan center to analyze the progress and get her feedback. She is regularly being motivated to visit her treating doctor. Preventive, promotive, and curative advice was given. Periodic examination and follow up were scheduled.
The patient is fully satisfied with the counseling and treatment of Medicine Department SRMSIMS. She has joined the short computer course. Now, she is feeling confident and happy. Her complaints have also disappeared. Symptomatically she seems to have been relieved of her complaints.
Case study 3
Patient : Hello, Doctor.
Doctor : Hello, please have a seat. What’s your name? Where are you from, and what do you do?
Patient : My name is ABC, and I’m from XY village. I have a shop.
Doctor : Alright, tell me how you ended up here and what problems you’re facing.
Patient : Doctor, I’ve been experiencing a lot of knee pain, difficulty walking, and a cough for the past two weeks. I’m quite troubled by it.
Doctor : Who referred you here?
Patient : Your SRMSIMS telemedicine bus came to our village. They provided me with some medication and instructed me to go to VARDAAN CENTER, near gate number 2, for further help. So, I came here.
Doctor : No problem, you’ve come to the right place. Your treatment will be done properly now. Have you been to any other place before this?
Patient : Yes, we’ve been to SRMSIMS twice before. It’s a big hospital, with a lot of people and long queues. We got confused, as nobody properly guided us on what to do, where to go, or whom to see. We were very distressed and returned home.
Doctor : What happened next?
Patient : We have a local doctor in our neighborhood. We consulted him, spent money, but didn’t find relief. Then we saw your bus and came directly here.
Doctor : Alright, please register yourself, and give me the yellow form.
Patient : What’s the significance of the yellow and white forms, and how do they help?
Doctor : The yellow form is for our documentation, and the white form is attached to your registration slip. Whenever you come here, bring both. It helps you get a 10% discount on prescribed medicines, 10% discount on lab investigations, and a 15% discount on bed admissions. Nursing staff and ward boys will assist you. MSW telecallers from Vardaan Center will contact you every 3 days to inquire about your condition and any problems you might have.
Patient : What other assistance will they provide?
Doctor : A nursing student or ward boy will take you to the OPD and help you with the paperwork. This saves your time, as you won’t have to stand in long queues or wander around. After your visit, return here and provide your feedback and experiences.
Doctor : Your satisfaction is our priority.
Patient : Thank you very much to your Vardaan Center. With your facilities, the doctor examined me comfortably, and I didn’t face any issues. I felt really good coming here. When should I visit the doctor again?
Doctor : The doctor has called you for a follow-up in 5 days. Please return, and bring this form with you.
Patient : Okay thanks so much;Bye doctor.
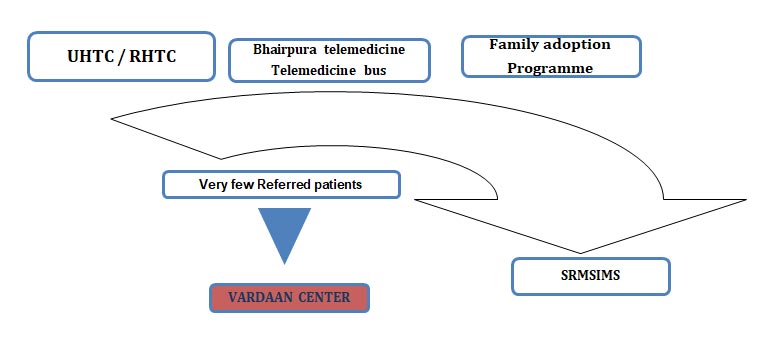
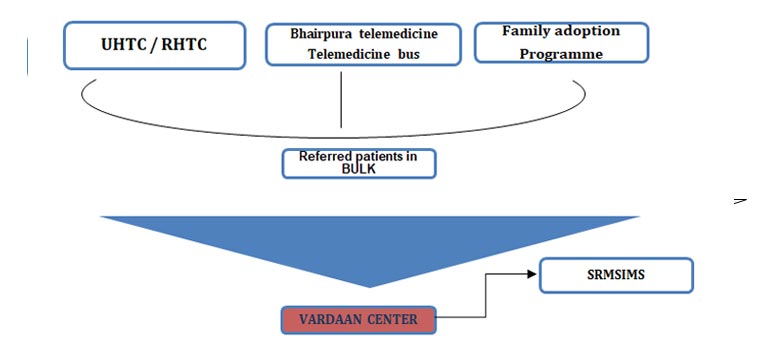
Currently, very few patients are coming to SRMSIMS through Vardaan. Mostly, they directly reach the hospital OPD (fig. 1). Against this background, meeting was held in the department with an objective to increase footfall in Vardaan center. It was decided that bulk of the patients from our field areas need to be routed to SRMSIMS through Vardaan center (fig. 2)
Discussion:
Referral has been described as a process in which a health worker at one level of the health system, having insufficient resources (drugs, equipment, skills) to manage a clinical condition, seeks the help of a better or differently resourced facility at the same or higher level 1,6,7. Less than 20% of sub centers, primary health centers & community health centers meet Indian Public Health Standards; 80% of them fall short of Gynecologists, Pediatricians and Physicians6.So, it is essential to have a sound referral system, to fulfill the existing gaps in health infrastructure. Health care systems of every country encourage patients to first attempt to get care at the primary level, and then to approach a higher level of care according to the need. This protocol minimizes the costs for the caretaker/patients. However, in most of the countries, patients often bypass primary care facilities and directly go to the higher center thereby, increasing the burden on higher level facilities.
For a referral system to be effective there must be clarity of role of every level of health care system. Appropriate communication and transport facility should be there. Adherence of health workers and patients to available standard operative procedures for appropriate referral and follow up care protocols should be ensured.
Initiating facility should have a protocol of care for various diseases. There should be adequate facilities for treatment and stabilization of patients. There should be an outward referral form available with arrangement of communication with receiving facility. Information should be provided to the patients and their caregivers regarding the reasons of referral; risks of non-referral; location of receiving facility; transport. Referral register should be there to monitor follow-up and to gather statistics.
At the receiving facility, arrangements should be there of anticipating patients’ arrival and providing appropriate care. A back referral form should be there with feedback to initiating facility on appropriateness of referral. Monitoring / quality control of outward and back referrals should also be there. Regular training for health staff may be arranged for making the referral system to be effective.
Back-referral system involves health service provision for patients with the stable chronic disease still needing treatment or long-term nursing care at primary health care level on the recommendation/reference from a hospital doctor6.
Health care system of India is plugged by: overpopulation, lack of expert clinicians, skewed distribution of physicians, lack of motivation among existing health care personnel and an ineffective referral mechanism1-4. Tertiary medical care institutions are expected to function as referral institutes. However, the doctors in the OPDs are usually overworked due to the large number of patients they have to attend. Many of problems of the patients reporting at OPD can be handled / resolved by a nurse/ counselor by non-medicinal interventions, e.g., appropriate behavior therapy, exercises, health education, counseling and guidance.
Given the prevailing scenario of referral system in India, much of the time of specialist doctors is wasted in attending to the routine problems/queries of patients. Consequently, they have no time or patience to explain these things to the patients. So, more or less, a lip service is given in OPDs during patient management to conservative modalities. Moreover, it is often seen that not much attention is given in the hospitals on emphasizing upon the patients and their relatives about the importance/effectiveness of the conservative management of various maladies.
In fact, the health promotion principle demands that a health culture needs to be developed among the public that many of their medical problems can be tackled even without any medicine/tablet/capsule/injection or surgery. Such cases need to be weaned off their habit/dependence on drugs or medicinal cure. Human body’s power of self-healing needs to be strongly emphasized. The concept of salutogenesis needs to be popularized. When such an image of behavior/conservative therapy is propagated through an apex institution like SRMSIMS, it carries a lot of weight. Such a move will help in creating a favorable health promoting culture as indicated above. Setting up a multipurpose behavior therapy room in Vardaan center, SRMSIMS, will be an effective step in this direction. This is the need of the hour.
There is an inherent element of de-medicalization in this approach. This will attempt to reduce the dependence of patients on doctors/medicines. Need of direct consultation with doctors will also be reduced. Simultaneously, this will help to instill a sense of confidence among patients and their caregivers. When they will observe the positive results of their taking charge of their own health, their concept of self-efficacy will improve.
The time of the doctors is also wasted when the dis-satisfied patients keep pestering them with un-necessary queries (because they were not explained about their problem at the first instance). In fact, a lot of consultation time of doctors can be saved if someone else deals with imparting such an advice to the patients. Thus, in this proposed Vardaan center, SRMSIMS approach, the OPD doctor will prescribe appropriate conservative therapy to the patient and will refer the patients to the staff in Vardaan center. This team will provide the behavior therapy and appropriate counseling to them. A continuity in the patient support will be ensured by establishing the linkage with the teams of our field practice areas. This way the back-referral system concept will help to provide doorstep self-care guidance to the patients and their families.
Work process at the Vardhan centre involves- counselling the referred patients for seeking appropriate treatment; ensuring patients’ satisfaction and feedback; saving patient’s time, money and unnecessary physical harassment; and protecting the patients from hazardous quack treatments. It focuses upon improving the communication between the patients and the health system.
Our data reveals that the back-referral system concept can be operationalized in teaching hospitals through outreach centre of Community Medicine departments. The three case studies conducted by us show that the patients were satisfied with the counseling and treatment provided through the Vardaan centre.
Author’s Contribution statement:The study was conceptualized and the methodology was developed by RA. RA also supervised the entire study and prepared the original draft. SSB was responsible for data collection and analysis and contributed to the writing, review, and editing of the manuscript. AS contributed to the interpretation of data and critically revised the manuscript for important intellectual content. All authors have read and approved the final manuscript.
Funding:No funding was taken for this study from any source.
Ethics Approval and Consent to Participate:Ethical approval for this study was obtained from the Institutional Ethical Committee of Ram Murti Smarak Institute of Medical Sciences (SRMSIMS), Bareilly. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee.
Consent for Publication:Informed consent for publication of the data was obtained from all individual participants included in the study.
Availability of Data and Materials:The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflict Interests:The authors declare that they have no conflict of interests.
References:
- Global strategy for health for all by the year 2000, Switzerland, Geneva,1981. www.WHOorganization.in
- Bashar MA, Bhattacharya S, Tripathi S, Sharma N, Singh A. Strengthening primary health care through e-referral system. J Family Med Prim Care 2019;8: 1511-3.
- Bhattacharya S. Health system strengthening‑ Focusing on referrals: An analysis from India. JOJ Nurse Health Care 2017;2(4):555592.
- Guideline For Implementation Of A Patient Referral System Medical Services Directorate;Federal Democratic Republic Of Ethiopia Ministry Of Health; May 2010 Addis Ababa, Ethiopia
- National Medical Commission Act, 2019
- Indian Public Health Standards‑Governnment of India.2019 Mar 02. http://www.nhm.gov.in/nhm/nrhm/guidelines/indian‑public‑health‑standards.html
- WHO | Hospitals.WHO.2019 Mar 02. http://www.who.int/hospitals/en/.
- Sharma R, Dhaliwal LK, Suri V, Kaushal P, Singhal N, Rana AK & Singh AJ. implementing a Life Cycle Approach through Establishment of a Multipurpose Behavior Therapy Room in PGIMER, Chandigarh for Enhancing the Fitness Level of Women. JPMER, 2017; 51: 115-122


